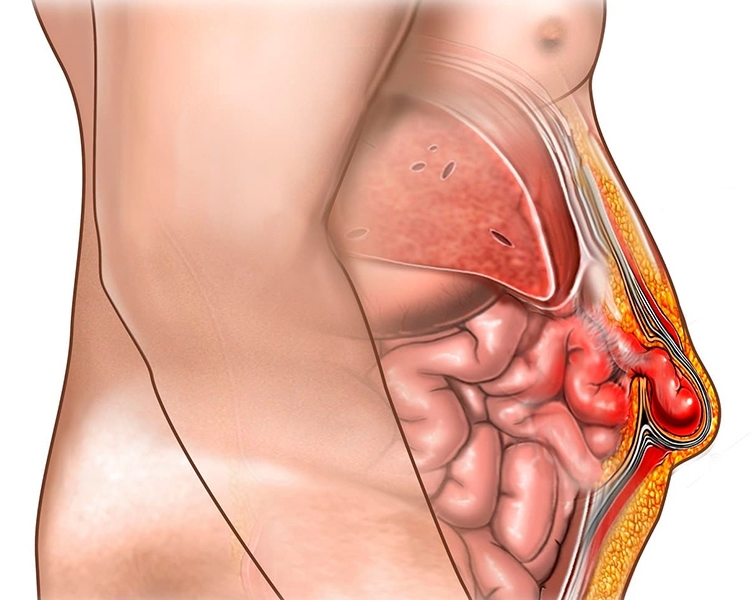
The compression of intra-abdominal organs in weak areas along the abdominal wall or in the area where the integrity of the abdomen is disrupted, that is, where there is a tear, is called abdominal hernia. The most common type is umbilical hernia, i.e. umbilical hernia, and the surgical site, i.e. incisional hernia, is encountered in 15-20% after surgeries.
Especially the increase in intra-abdominal pressure is important in the development of hernia. Especially umbilical hernia is common in women and increases with pregnancy. Family history of hernia, heavy physical activity, muscle and connective tissue diseases and old age are among other causes. The incidence rate of incisional hernia after open abdominal surgery is around 20% and especially obesity, cancer surgery, smoking, heart, lung and diabetes increase these risks up to 40-50%.
Although the symptoms vary according to the compressed organ, swelling and pain are the most common symptoms. Especially intestinal obstruction develops as a result of compression of the intestines in the hernia and has a high life risk.
As in every disease, a good physical examination is the first step in diagnosis. In addition, imaging methods such as ultrasound and tomography can determine the size of the hernia, the compressed organ and changes in this organ.
People who are diagnosed with gastroscopy can undergo computed tomography or PET scan to get information about the spread.
The definitive solution of hernia is surgery. In surgeries performed using patches called mesh, the compressed organ is examined. If there is no problem in this organ, surgery is performed by pushing it into the abdomen and placing a patch in the hernia area.
Laparoscopic hernia surgery is more advantageous than open surgery due to the evaluation of the intra-abdominal organs and the placement of the patch between the muscles. In addition, less bleeding, less use of painkillers, shorter discharge and early return to daily life are also possible with laparoscopic hernia surgery.


