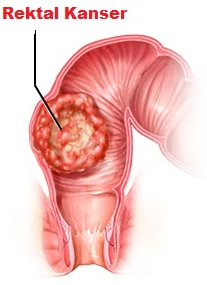
The rectum is the last part of the large intestine and especially provides the storage of large ablution. 1/3 of large intestine cancers are seen in the rectum. As in colon cancer, the change that starts with polyps progresses to cancer.
Especially people with genetic and family history, smoking, alcohol use, animal fatty diet, smoked and processed food consumption and inflammatory bowel diseases such as ulcerative colitis, crhon and most importantly people with a history of cancer in close relatives are in the risk group.
In particular, haemorrhage and associated low blood counts are the most common symptoms. Patients who have a change in their stool habits, i.e. diarrhoea and constipation, notice changes such as mucus in the stool. Especially unexpected weight loss is also a warning for us.
Weight loss is the most important symptom and the patient should be evaluated with further examination without losing time.
The most important imaging method in diagnosis is colonoscopy. Both the biopsy is taken and the remaining large intestine is checked at the same time. Sometimes polyps are seen in the remaining large intestine and these polyps are removed by colonoscopy and sent to pathology. The pathologist examines the polyps under a microscope and depending on the degree of the polyp, only polypectomy will be considered sufficient or an additional intervention is determined.
In laparoscopic surgery, i.e. surgery performed by closed method, depending on the location of the cancer, sometimes permanent bag opening, in which the anus is permanently cancelled, may be necessary. If the cancer is located 3-5 cm above the anus, the intestines can be reconnected to each other.


