What is Haemorrhoids?
The discomfort caused by enlarged, that is, swollen blood vessels that have lost their natural characteristics in the last part of the anus is called haemorrhoids. Disease-free haemorrhoidal veins, i.e. anal pads, are actually structures that help us to hold gas escape and liquid stools. The muscular structures (collagen fibres) in the anus start to loosen and sometimes break down in the 40s and as a result, the anal pads slip out of their places and hang out. The 3 anal pads can be pressed by faeces, causing blockage of blood vessels and bleeding. With the addition of inflammation, haemorrhoidal disease occurs. Depending on the degree of the disease, these vessels may protrude intermittently or continuously from the anus.
Who is it commonly seen in?
Wrong eating habits cause many disorders in our gastrointestinal system. Among these, haemorrhoids are the most common disease we encounter. In adulthood, 80-90% of people have encountered this disease at some point in their lives. Again, low water consumption, spending time in the toilet for a long time (the most common reason for this is the desire to play social media or games with the phone in hand), constantly working in a sitting position, old age, pregnancy, a life away from exercise and obesity are among other reasons that we encounter.
What are the Symptoms?
As there is no problem in simple haemorrhoids in patients, there are problems such as non-stop bleeding, discharge, itching in advanced patients. Haemorrhoidal diseases appear in 4 degrees for internal haemorrhoids. Symptoms vary according to the degree of the disease. In external haemorrhoids, pain is at the forefront due to the rich nerve network. Haemorrhoids that have developed thrombosis as a result of clots are the most intense period of pain.
- Grade: It is the first grade with intermittent bleeding. It is usually detected during endoscopy.
- Grade: It is the period when itching is accompanied. It is noticed during the examination, particularly during straining. Haemorrhoids, which come out during defecation, enter inside spontaneously after defecation. Pain is present during defecation.
- Grade: It is the period when pain and wetness are felt from the anus. Bleeding and itching are increased. Haemorrhoids that do not enter spontaneously can be sent in manually during examination. Pain is also present during and after defecation.
- Grade: It is the last stage of haemorrhoids and the haemorrhoid nipples that comes out cannot be sent inside during the examination. Bleeding, pain and discharge are extremely common. In every patient with bleeding, the anus area should be examined by endoscopy and it should be checked that other causes such as cancer, inflammatory bowel disease, diverticular diseases are not accompanied.
In every patient with bleeding, the rectal area should be examined with endoscopy and it should be checked that other causes such as cancer, inflammatory bowel disease, diverticular diseases are not accompanied.
How is the diagnosis made?
The patient’s complaints and examination give us information about the degree of the disease. In advanced disease and severe bleeding conditions, the rectal area should be examined by endoscopy with the help of a camera and the diagnosis should be made. It should not be forgotten that what is underlying the rectal bleeding may always be cancer.
How is it treated?
In stage 1-2 patients, nutritional regulation and treatment with medication are generally prioritised. In stage 2 patients with a tendency to progress, early surgery is used to stop the progression of the disease and control bleeding and pain. In stages 3 and 4, the only treatment is surgical intervention, and particularly in stage 4 haemorrhoidectomy with stapler is frequently applied.
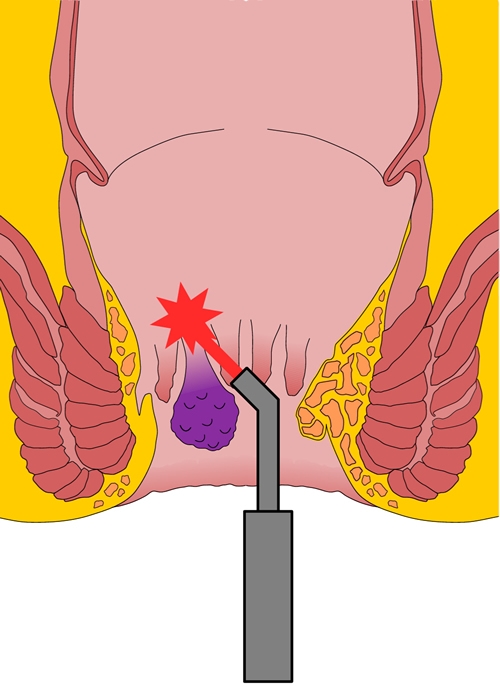
What is Treatment with Laser?
Laser treatment is possible in stage 3 and advanced stage 2 haemorrhoids. With laser, hemorrhoidal cushions are extinguished with heat from the inside and there is no sagging and foreign body use and there is no narrowing in the anus. Since the incision and stitching process applied to the patient in classical surgery does not exist in the laser, pain, bleeding and loss of labour force are minimised.
How long does the treatment take?
After classical surgery, patients return to their daily lives within an average of 2 weeks, while this period is longer in surgeries performed with stapler. In laser interventions, the patient returns to daily work on the same day.
What is the Chance of Recurrence?
Recurrence rates after haemorrhoidectomy with ligasur and stapler are between 4.5% and 18.8% and the risk of recurrence is similar in laser treatment.
Post-Treatment Control and Diet
Nutrition and toilet habits are the methods that particularly affect the possibility of recurrence of the disease the most. We recommend that our patients should be fed with liquid and fibrous foods and we want them to spend the least time possible in the toilet. Sitting on the toilet for a long time and straining particularly increases the possibility of recurrence.


